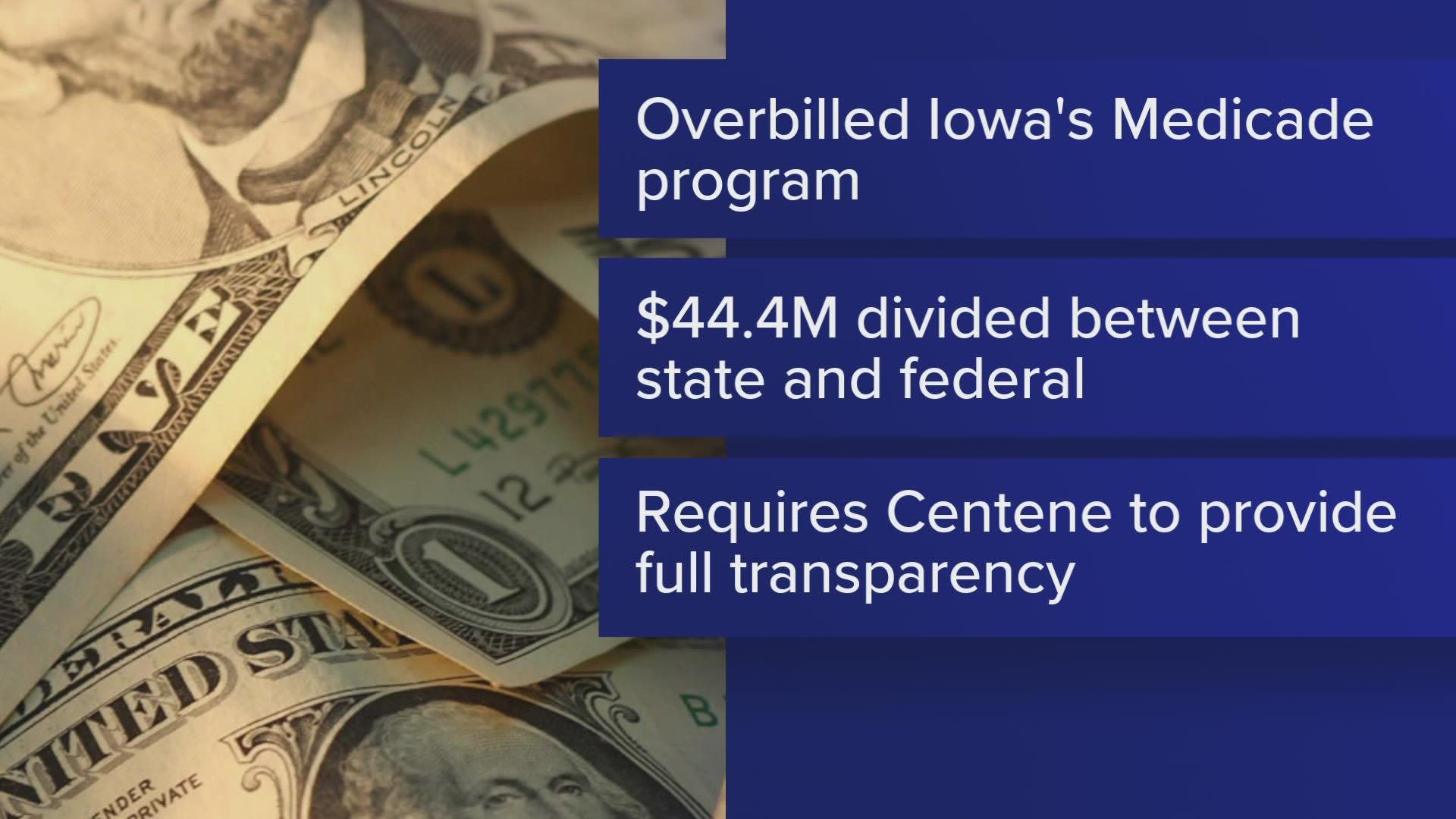
DES MOINES, Iowa — Iowa Attorney General Miller announced Thursday the state will receive $44.4 million in a settlement with Centene Corporation, a managed care organization.
According to a press release from the AG's office, the settlement follows allegations that the company overcharged Iowa’s Medicaid program for pharmacy benefits and services.
The money received from the settlement will be divided between the state and the Federal Medicaid program in accordance with federal Medicaid requirements.
“Medicaid funds are a vital resource for so many Iowans. Ensuring these dollars are used as intended means that our health care system is in a better spot to help our residents,” Miller said in a statement.
The managed care corporation operates as Iowa Total Care, one of three managed care organizations under the state’s Medicaid program.
Miller’s office reviewed Centene after investigations from other states.
The review found inconsistencies in the company's reporting of pharmacy benefit costs within the Medicaid program as well as in the pricing of prescription drugs.
Iowa Total Care uses Centene-owned pharmacy benefits manager Envolve, where the corporation allegedly misrepresented costs of services, falsified reports and receive unwarranted payments.
According to the statement, the settlement requires Centene to provide full transparency surrounding the payment of all pharmaceutical benefit claims.