DES MOINES — The Iowa Department of Human Services (DHS) announced on Wednesday that contract negotiations with the state’s Managed Care Organizations (MCOs) have concluded and contracts have been signed for State Fiscal Year 2020 (SFY20).
See the contracts here.
New protections, according to DHS, are included in the contracts for Long-Term Services and Supports (LTSS) members. These protections include key requirements related to the level of care assessments to ensure additional quality oversight for LTSS members. Additional protections have also been added for providers related to credentialing and claim payment system issues.
The 8.6% increase announced Wednesday will include $115 million in additional state funding, with the federal government paying for the remaining portion.
The $5 billion Medicaid program serves about 600,000 poor and disabled people.
DHS says the rates include changes made by the Iowa Legislature, which account for about 2 percent of the increase. Last year the agency approved a $344 million increase over the previous year.
“Medicaid members and providers can be assured that both, Amerigroup and Iowa Total Care, are here to serve Iowans for the long term. These new contracts demonstrate a commitment to those we serve including greater access to Hepatitis C treatment and additional funding for the adult mental health and children’s mental health systems,” said Medicaid Director Michael Randol.
Under the new contracts, Iowa will be increasing Medicaid funding by 6.5%.
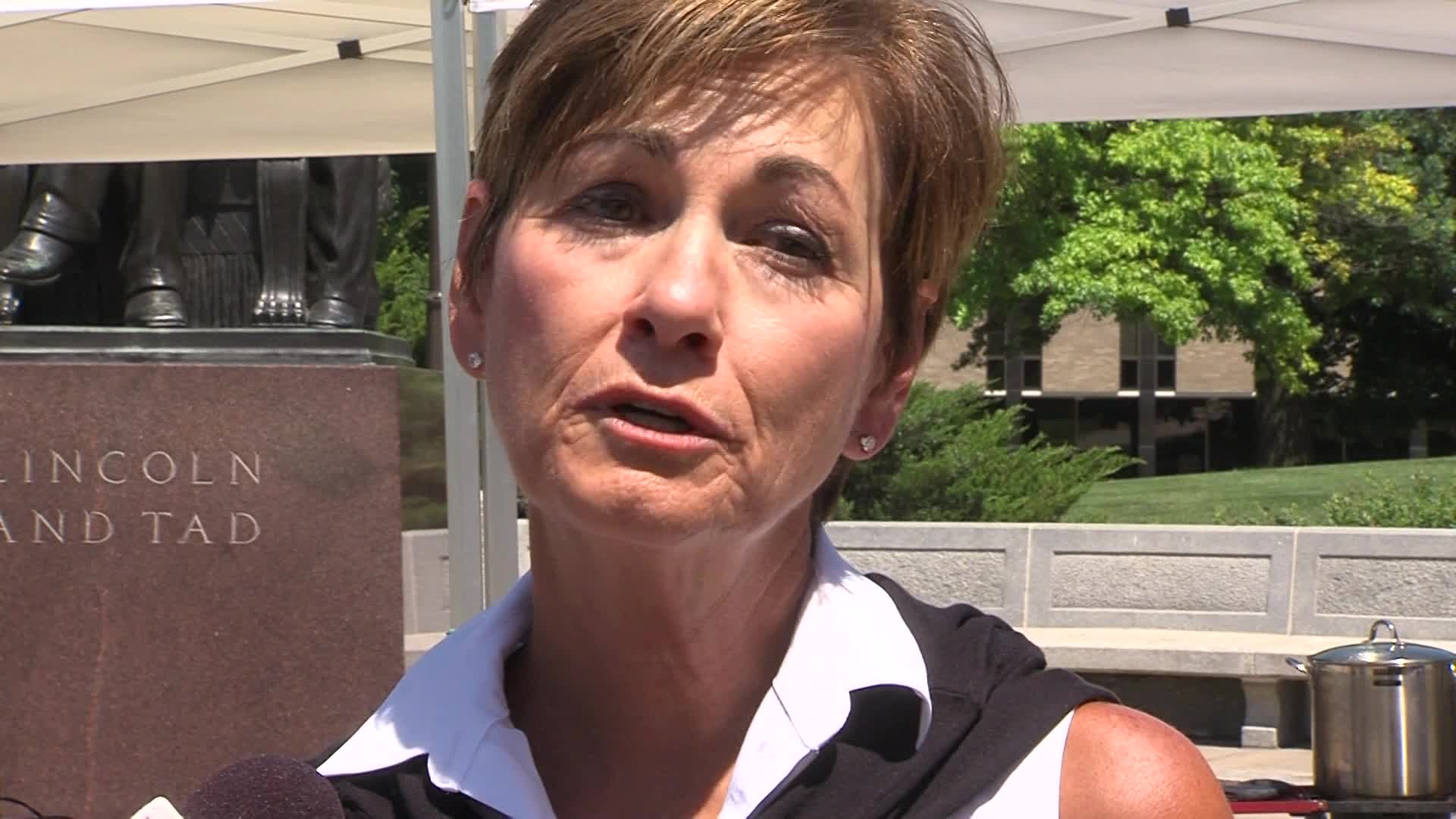
“With additional funding for nursing homes, mental health services, and health care providers, this agreement provides Iowans compassionate, integrated, and coordinated health care options. The negotiated contract ensures greater health care access for those who need it and demands more accountability from the managed care organizations involved in the program,” said Gov. Kim Reynolds.